Artificial intelligence is rapidly reshaping healthcare — from how doctors document visits to how hospitals manage patients and resources. In late 2025, that transformation took a major political turn when a new healthcare and budget bill championed by President Donald Trump began financially incentivizing the use of AI in healthcare, particularly in rural America.
Supporters say the move could modernize a struggling system. Critics warn it could introduce serious risks if speed outpaces safety.
Here’s a clear, comprehensive look at what this policy means, what often gets overlooked, and why experts are urging caution.

What the Healthcare AI Incentive Actually Does
At the heart of the legislation is a multi-year Rural Health Transformation Fund, designed to encourage states to adopt advanced technologies — including AI — in rural hospitals and clinics.
To qualify for funding, states must show progress in modernizing healthcare delivery through tools such as:
- AI-assisted clinical documentation
- Predictive analytics for patient care
- Remote monitoring and telehealth systems
- Automation of administrative tasks
The stated goal is to improve access and efficiency in regions facing severe provider shortages. However, critics argue that the funding may not fully offset other healthcare cuts within the same bill, particularly those affecting Medicaid — a key lifeline for rural hospitals.
Why This Policy Matters Beyond Rural Hospitals
This bill is not an isolated move. It reflects a broader “AI-first” strategy shaping federal policy:
- Faster adoption over cautious regulation
- Reduced barriers for testing and deploying AI tools
- A strong emphasis on U.S. technological competitiveness
Healthcare has become a proving ground for this philosophy — and the consequences could affect every patient, not just those in rural communities.
The Promise of AI in Healthcare
When implemented responsibly, AI offers real benefits:
1. Less Burnout for Clinicians
AI can automate clinical notes, billing codes, and scheduling — freeing doctors and nurses to spend more time with patients.
2. Better Support for Underserved Areas
Remote monitoring, AI-powered triage, and virtual care tools can extend care to communities with few specialists.
3. Improved Operational Efficiency
Hospitals can use AI to optimize staffing, predict patient flow, and manage supplies more effectively.
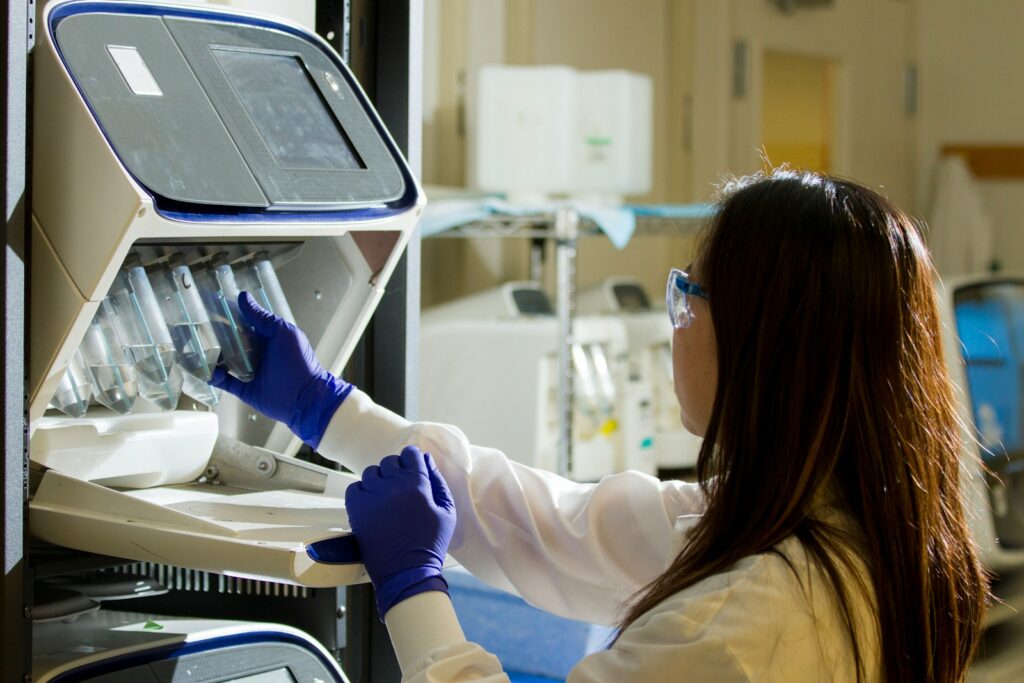
4. Smarter Clinical Decision Support
AI can flag anomalies in scans, lab results, and health records, serving as an extra layer of insight — not a replacement for clinicians.
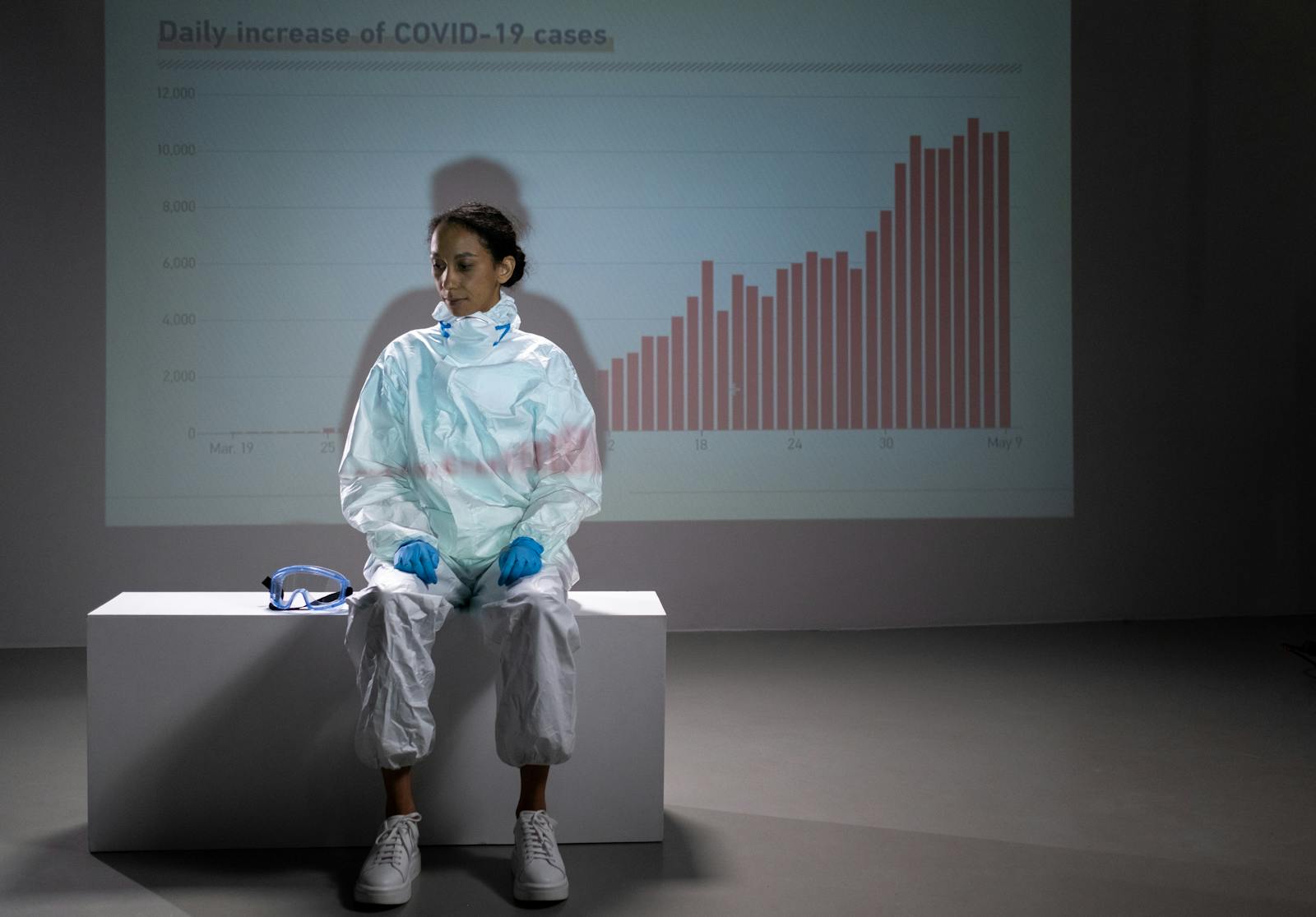
Why Experts Are Sounding the Alarm
Despite the promise, healthcare professionals, researchers, and patient advocates urge caution.
1. Patient Safety Comes First
AI systems still struggle with nuance, rare conditions, and complex clinical judgment. Over-reliance could lead to misdiagnosis or delayed care if safeguards are weak.
2. Privacy Risks Are Growing
Healthcare AI relies on massive amounts of sensitive data. More data sharing means more potential entry points for breaches, misuse, or unauthorized access.
3. Bias Could Worsen Health Inequities
If AI is trained on incomplete or biased datasets, it may underperform for minority and marginalized populations — reinforcing existing disparities instead of reducing them.
4. Workforce Readiness Is Uneven
Many clinicians have little formal training in AI tools. Without education and oversight, adoption could be inefficient — or dangerous.
What’s Often Missing From the Debate
Most coverage focuses on innovation, but several critical issues receive less attention:
- Ethical Oversight: Who is accountable when AI makes a harmful recommendation?
- Transparency: Patients often don’t know when AI is involved in their care.
- Long-Term Costs: AI systems require maintenance, updates, and cybersecurity investments.
- Small Hospital Strain: Rural providers may struggle to implement AI without technical support.
AI isn’t “plug and play.” Without infrastructure and governance, incentives alone may fall short.
What the Future of Healthcare AI May Look Like
If current trends continue, the next few years could bring:
- AI assistants embedded into electronic health records
- Automated patient intake and triage systems
- AI-supported chronic disease management
- Greater integration between telehealth and in-person care
- Stronger calls for national standards on safety, fairness, and accountability
The central question isn’t whether AI will shape healthcare — it already is. The question is how responsibly it will be deployed.
Frequently Asked Questions
Is AI required to make medical decisions under this policy?
No. The incentives encourage adoption of AI tools, but medical decision-making still legally rests with licensed clinicians.
Will this improve healthcare in rural areas?
It could — especially for access and efficiency. However, success depends on proper funding, training, and infrastructure.
Should patients worry about privacy?
Patients should remain informed. AI systems process large volumes of data, making strong security and transparency essential.
Could AI replace doctors or nurses?
Unlikely. AI is designed to assist, not replace, human clinicians. The greatest value comes from collaboration between humans and machines.
What safeguards are needed moving forward?
Clear regulations, bias testing, clinician training, patient consent transparency, and accountability frameworks are all critical.

Final Thoughts
AI has the power to improve American healthcare — but only if innovation is matched with responsibility.
Trump’s healthcare bill accelerates adoption, especially in rural communities that need support. Yet experts warn that speed without safeguards could compromise patient trust, equity, and safety.
Healthcare isn’t just another industry. When AI enters exam rooms, lives are at stake. The success of this policy will depend not on how fast AI is adopted — but on how wisely it’s used.
Sources The Guardian